by Mark Craddock
OUR WORLD — Last week, Las Animas-Huerfano County Public Health Department’s Robert Bukovac drove to an undisclosed location somewhere in a five-county region.
He took Huerfano and Las Animas counties’ share of personal protective equipment being distributed from the national stockpile.
It wasn’t much. The haul fit comfortably in his car, with room to spare.
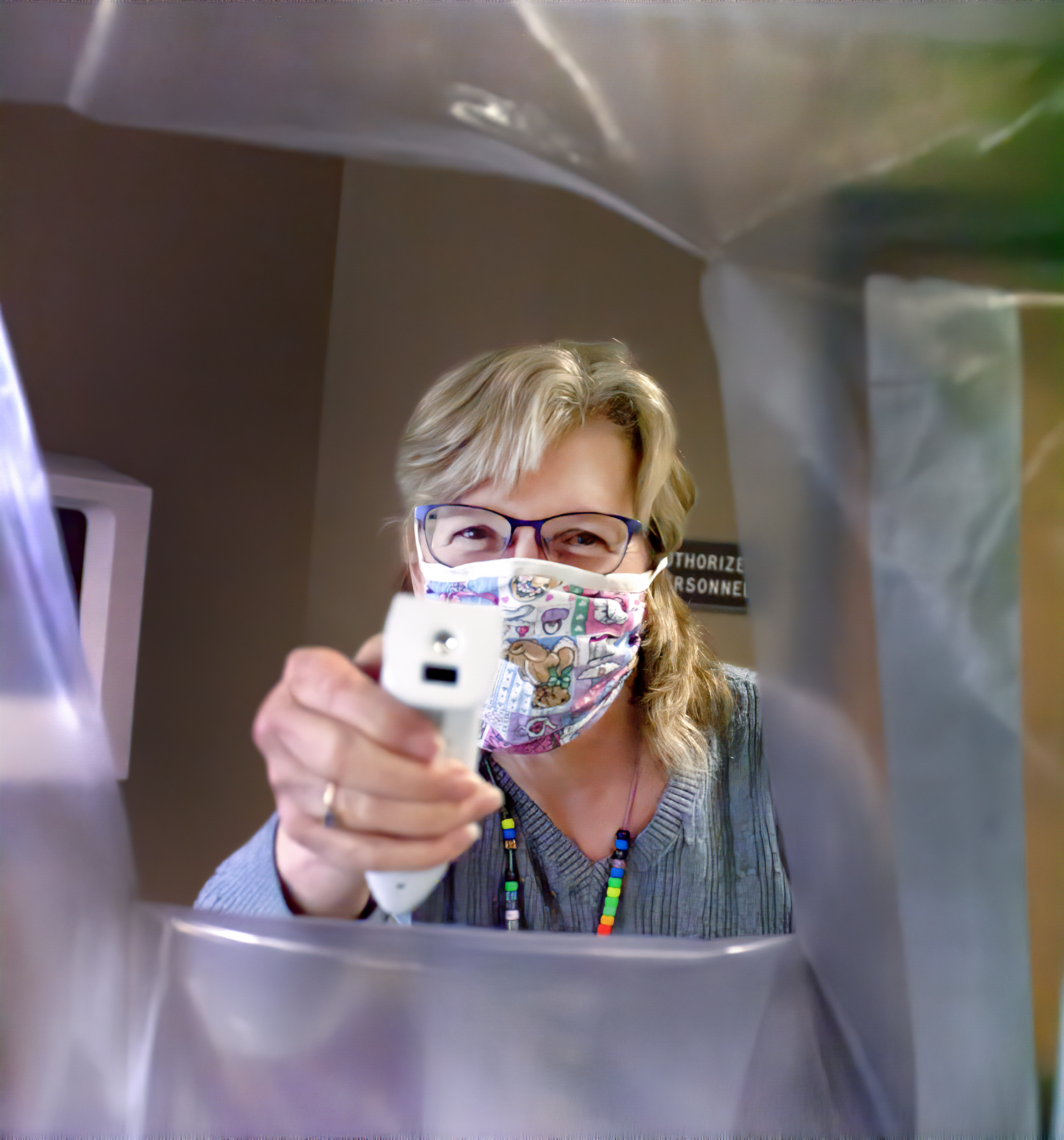
Meanwhile, Nancy Christensen sat at her sewing machine.
For days, she had been turning roughly 11 square feet of tightly woven cotton cloth and about 14 inches of elastic into surgical masks. Christensen, Jaye Sudar, Patti Davis and several dozen like-minded peers have churned out hundreds of these home-brew masks for donation to the Spanish Peaks Regional Health Center, PIO Debbie Channel said.
The homemade masks are a hit at the hospital. Some feature decorative designs on the fabric, some are actually crocheted, with a cloth lining. Some have elastic bands, others tie on to the user. One creative mask maker used pipe cleaners at the bridge of the nose and another built a mask that holds disposable paper coffee filters for extra protection.
The bi-county health department has launched a community donations drive, hoping area businesses and organizations may have some safety gear in inventory.
And Huerfano County’s entrepreneurial success-story, Chaé Organics, which manufactures a line of organic cosmetics and skin-care products, is pumping sanitizer out by the gallon, donating it to regional health and safety organizations.
Hope for the best, prep for the worst
With Colorado in statewide lockdown and paltry COVID-19 testing in rural Colorado leaving local communities in the dark about the true nature of their COVID-19 risk, rural health care facilities are doing whatever they can to brace for a surge of patients they hope will not come.
And securing adequate amounts of personal protective equipment is becoming an increasingly difficult task.
Representatives from the region’s three hospitals – Mt. San Rafael in Trinidad, SPRHC in Walsenburg and Miners Colfax Medical Center in Raton – all report adequate supplies to handle day-to-day operations.
What frightens them is a sudden surge of patients.
“We’re preparing for the unknown. That’s really difficult.” Debbie Channel, SPRHC spokesperson, said.
“My goodness. Put your head down and hang on,” said Jo Greene, public information officer at Miners Colfax Medical Center in Raton.
“We’re holding our own, but being very strategic” Kim Lucero, director of planning and development, at Mt. San Rafael, said.
“Certainly there’s going to be a point where we do not have enough (PPEs) if this thing blows up,” Channel said. “Right now we have a decent stock – not great, but decent. I can’t say there’s 100 percent of anything, because there are so many unknowns.
SPRHC, which shares a campus with a state veterans nursing home, is particularly sensitive to a COVID outbreak of the kind that have swept through the vulnerable populations in several nursing homes both in Colorado and nationwide.
The facility has barred visitors from the nursing home, and is screening both the public and staff upon entering and leaving the building. She said a recent El Pomar grant will go toward purchasing a UV sterilizer, which can be used to sanitize small personal items like wallets and shoes, when someone enters the building.
At Trinidad’s Mt. San Rafael Hospital, Lucero largely mirrored her Walsenburg counterpart.
“We’ve got some orders placed,” Lucero said, “ but it’s hard to estimate how much we will need.” She said Mt. San Rafael has a step-down unit, which provides an intermediate level of care between an intensive care unit and the general medical wards.
She said the hospital has at least three ventilators and one negative-pressure room.
Lucero said the hospital has seen no COVID patients yet and hopes that stay-at-home orders and social distancing may spare local hospitals from the brunt of the pandemic.
“This is not a vacation for people,” she said. “If people follow the governor’s orders, it should work.”
At MCMC in Raton, Greene said the facility is doing “everything possible to keep our workforce and our community safe.”
She said the hospital has activated its emergency preparedness plan and incident command system. In keeping with New Mexico public health orders, the hospital has suspended all non-essential healthcare services to preserve PPE. And the hospital has restricted visitation to both the acute care hospital and the long-term care facility.
“Currently, MCMC has adequate medical staff, equipment, beds, PPE and resources to respond in the event known cases of COVID19 are identified locally,” Greene said. “Additional resources for PPE and medical supplies are being requested and orders being received subject to manufacturer availability.”
“Our biggest concern now is the nationwide shortage of test supplies and materials.” she said.
Greene did not respond to questions regarding the number of intensive-care units and ventilators at the facility, the average number of available beds – or even the total number of beds in the hospital.
PPE shortages abound
With demand far outstripping supply nationwide, with orders of various PPE going unfilled and bidding wars erupting among governmental agencies, it is hard to tell when or if orders from any local facilities might be filled.
When Gov. Polis announced the state received PPE from the national stockpile, he admitted it would amount to little more than a one-day supply for the state’s hardest-hit hospitals.
Bukovac, emergency preparedness and response coordinator for Las Animas-Huerfano Counties District Health Department, said the local share broke down as follows:
SPRHC received one case (96 ct.) of face shields; a case (240 ct.) of N95 masks; a case (500 ct.) of surgical masks; and 144 gowns in various sizes.
Mt. San Rafael Hospital received two cases of surgical masks (1,000 total); two cases of face shields (192 total); three cases of N95 masks (720 total); and six cases of gowns. He said the health department also disbursed a small amount of supplies to area emergency workers.
Bukovac said surge capacity at both local hospitals is low, and a rush of COVID patients would almost certainly bring them to their knees. Neither hospital has ICU beds, he said, and the number of beds in general is quite limited. Serious patients are routinely transferred to Pueblo.
He used Mt. San Rafael, the larger of the two hospitals, to make his point.
“I think they only staff 15 beds here in Trinidad. A lot of times those are filled already,” he said. “You’ve got your normal people sick and your beds are full and you get 30 people showing up to the emergency room. That’s a problem.”
Send in the Army Corps
According to a Monday, March 30, release from the State Emergency Operations Center, it is working with the Army Corps of Engineers and communities statewide to increase the number of intensive care beds.
Current estimates are that Colorado has a total of 1,849 ICU beds. The state’s goal is to add 1,000 beds by May, and another 5,000 by the summer.
In the meantime, each health care facility is working to move patients out of ICUs, when possible, into acute care beds and lower-needs beds in order to prepare for increased demand in ICU settings.
Local public health organizations and local emergency managers are also working to identify alternative care sites, the SEOC says.
In addition to medical sites, the SEOC is working with the Army Corps to identify other locations like hotels, dormitories and vacant buildings that could potentially be repurposed for medical use.
Bukovac conjectured that a regional site in, say, Pueblo may be constructed to handle surge capacity for rural southern Colorado hospitals.
“You could funnel people not well enough to go home, but not sick enough for the hospital ICU, there,” he said. “I’m just speculating. But if you were to put an alternative care facility any place but Pueblo, it would tax the resources in every surrounding rural community.”